A Survey of Speech-Language Pathologists’ Knowledge and Perception About Their Role in Providing Dysphagia Services in India
Article information
Abstract
Purpose
Speech-Language Pathologists (SLPs) are frequently involved in dysphagia services including identification, assessment, diagnosis, and rehabilitation. Understanding of SLPs’ role in dysphagia care has evolved drastically in India over the last decade; however, research and advocacy are still in emerging status. In order to refine dysphagia practice patterns in India, we should understand the current standards. Thus, the present study was conceived to investigate SLPs’ knowledge and perception about their role in providing dysphagia services in India.
Methods
A cross-sectional online survey research design was employed. The survey questionnaire comprised of four sections that evaluated SLPs’ demographic characteristics, exposure to dysphagia services, self-perception about their role in the dysphagia rehabilitation team, and knowledge related to assessment and management of individuals with dysphagia. The obtained responses were stored in Google forms and were further analyzed in terms of percentage.
Results
A total of 269 SLPs responded to the survey and 59% of the respondent SLPs practicing in India were rendering dysphagia services. Although a majority of the SLPs had adequate knowledge and were aware of their role in the interdisciplinary dysphagia rehabilitation, they lacked opportunities to be a part of the team.
Conclusion
The survey clearly identified the trend and issues in dysphagia service delivery by SLPs in the Indian scenario by evaluating their knowledge and skills fundamental to the assessment and management of individuals with dysphagia. This further necessitates a re-examination of the role of SLPs in providing dysphagia services in India in view of establishing standard guidelines and practice patterns.
INTRODUCTION
Dysphagia is one of the primary areas of clinical practice for speech-language pathologists (SLPs), which can be tracked since the 1970s [1]. In the past decade, SLPs have taken a leading role in evaluating, diagnosing, and managing services for patients with dysphagia [2]. The evaluation may include bedside evaluations, in-patient, and out-patient assessments. The pertinent diagnostic information includes: (1) recognizing the causal factor that explains dysphagia, (2) developing a tentative hypothesis that describes the problem, (3) identifying any issues that would indicate additional testing, and (4) determining if the patient can tolerate further testing [3]. When required, they perform instrumental evaluation, which allows the visualization of anatomical structures and physiology of swallowing mechanism [4]. These comprehensive evaluations allow SLPs to formulate appropriate treatment plans and recommendations. Recognizing the significant potential impact of swallowing disorders on overall health and quality of life, SLPs must possess the knowledge and skills to be proficient in managing dysphagia. Depending on the individual’s work environment and population served, every SLP will not necessarily need to develop proficiencies in all roles. Some roles are clinical, and SLP will need to establish proficiencies based on the populations served (e.g., adult, head and neck cancer, pediatrics). Some roles are administrative and would be best performed by a person with extensive supervision experience. Broadly, SLPs are one of the chief service providers in the dysphagia interdisciplinary team. The level of expertise and achievement of proficiencies of SLPs who provide services to individuals with dysphagia should be documented, and systematic plans for attaining proficiency should be regularly re-examined [3]. Most often, survey methods are used in the literature to understand the level of SLPs’ competency in dealing with individuals with dysphagia. Survey research is a quantitative method for collecting information from a pool of respondents by asking multiple survey questions [5]. This research type includes recruitment of individuals, collection, and analysis of data. Such survey studies have covered broad aspects related to awareness, knowledge, and skills in dysphagia among SLPs.
Regardless of the increasing demand for SLPs to provide dysphagia services, there is little evidence on practice behavior. Only a few studies have surveyed SLPs regarding their dysphagia practice. A recent electronic survey was conducted in Canada to identify the trends and issues in dysphagia service delivery by SLPs [6]. This national survey endorsed the demand for dysphagia services and demonstrated that SLPs play a leading role in dysphagia care settings. Further, the extent of dysphagia training and workplace support available to SLPs in Malaysia and Queensland, Australia, was examined [7]. They explored clinicians’ perceptions of the training and support provided and their knowledge, skills, and confidence. Malaysian clinicians were found to have received significantly less university training, less mentoring in the workplace, and were lacking critical infrastructure needed to support professional development in dysphagia management. Over 90% of Queensland clinicians were confident and felt they had adequate dysphagia management skills; in contrast, significantly lower levels of knowledge, skills, and confidence were observed in the Malaysian cohort. The findings identified a need for improved university training and increased opportunities for workplace mentoring, training, and support for Malaysian SLPs. A survey was conducted on the clinical decision by SLPs in identifying swallowing impairments and determining treatment measures while they viewed videofluoroscopic swallows [8]. They found poor to a moderate agreement in swallowing impairment identification, frequent false positives, and wide variability in treatment planning recommendations. These suggested additional research and training in healthy and disordered swallowing are needed to increase accurate diagnosis and treatment among clinicians.
The role of SLP in dysphagia services is well described by international organizations [3]; it is not the same in the Indian context. A recent review study on dysphagia research in India reports that the role of SLPs in dysphagia practice is not well established, and it lacks research evidence [9,10]. This may be due to relatively less emphasis on this subject area during their academic learning, limited interest in the subject area, or confined exposure compared to medical professionals. A recent survey on dysphagia practice patterns among SLPs in India demonstrated considerable variability with barriers related to funding, availability and access to instrumental evaluations, and limited clinical training [11]. As this was a preliminary survey which included responses of 48 SLPs, generalizability of the results may be arguable. SLPs in India tend to determine their own protocols or adapt from the guidelines of practice established in other countries which might not match the culture-specific patient care. Thus there is a great need to establish national guidelines to improve the standards of dysphagia practice and quality of patient care suitable for Indian context. As dysphagia is an emerging topic of interest among SLPs in India, research evidence for understanding the role of SLPs in dealing with individuals with dysphagia is essential. Thus, the present study aimed to investigate the knowledge and skills possessed by SLPs to efficiently deliver services to individuals with dysphagia and further understand their perception about their role in the assessment and management of individuals with dysphagia. The survey served as a groundwork on realizing the extent of inclusion and involvement of SLPs in the interdisciplinary team of dysphagia assessment and management in India.
METHODS
Development of survey questionnaire
Questions to assess the knowledge and skills of SLPs in dysphagia and their perception about their role in the assessment and management of dysphagia were prepared in English language. These questions were developed based on the available questionnaires and published guidelines on dysphagia practice. The questionnaire was scrutinized for the content, relevance, comprehensiveness, and ease of administration by three practicing SLPs who had a minimum of five years of experience with dysphagia practice in India. Based on the feedback received which included minor grammatical revisions, the questionnaire was finalized. The questions were divided into four sections: Part A, Part B, Part C, and Part D (Supplementary information). Questions in Part A focused on demographic details of the respondents, including age, gender, nationality, qualification, work setting, the population that SLPs work with. The last question of Part A asked if SLPs worked with individuals with dysphagia. Those SLPs who reported to have worked with individuals with dysphagia were eligible to continue the survey by proceeding to the further sections. Part B comprised of five questions to assess SLPs’ exposure and experience in the field of dysphagia which included details on years of work experience, caseload, and specific training in delivering dysphagia services, if received any. Further, Part C had five questions to assess the necessity and involvement of SLPs in the assessment and management of individuals with dysphagia. Lastly, Part D assessed dysphagia-related knowledge of SLPs with 11 questions. This section included questions about the causes, assessment, associated conditions, team members, SLPs role, intensity of dysphagia therapy, and referrals. The response format included binary choice, multiple-choice, and short answers depending on the questions. These questions were fed into Google forms along with the required answer formats.
Data collection
A cross-sectional survey research method was employed to collect data from the participants. The survey link was circulated among practicing SLPs through emails and WhatsApp platforms. The survey was open to accept the responses for four months (December 2019 to March 2020). Snowball sampling was adapted to expand the participation. With this self-reported criterion, the eligible SLPs voluntarily participated in the online survey, and they were free to withdraw from the study at any time. An informed consent was recorded from all the respondents who participated in the survey. The participants had to have an experience of working with individuals with dysphagia, regardless of the work setting, to participate in the survey. Those who mistakenly participated in the survey were again asked if they had experience working with dysphagia at the end of Part A. Only those who had worked with dysphagia in their professional practice were requested to continue to participate in subsequent sections of the survey. After completion of all the sections, the participants were provided with an opportunity to express their comments or suggestions, if any.
Data analysis
The responses provided by the participants were stored on a Google form response sheet. The answers for each question in all the sections were coded and analyzed. Statistical Package for Social Sciences (SPSS) version 21 was used for statistical analyses. Descriptive analyses were carried out; the results of frequency analyses of the outcomes of the study were displayed in terms of percentages.
RESULTS
A total of 269 practicing SLPs responded to the survey and the results are presented below in separate sections. Virtual snowball sampling yielded around 7.4% of the total number of participants.
Part A: Participant demographics
The distribution of survey respondents by age and educational qualification is presented below. Among 269 survey respondents, 222 (82.5%) were between 21 and 30 years; 35 (12.9%) of them were between 31 and 40 years. 6 (2.2%) of the respondents were between 41 and 50 years of age. In the age ranges 51–60 and greater than 60 years, there were three participants (1.2%) each. On analyzing the educational qualification, the respondents had acquired related degrees such as Bachelors in Audiology and SLP (33.5%), Masters in Speech and Hearing (32.7%), Masters in SLP (21.2%), and Bachelors in Speech and Hearing (2.6%). The respondents included research scholars (4.5%), Ph.D. holders (2.2%), and post-doctoral candidates (0.7%). Given the experience in the field of SLP, 70.6% of the participants had 2–5 years of experience, 13.1% of them reported to have 6–10 years of experience, 11.9% were beginners with 0–1 years of experience, 2.2% had 11–20 years, and 2.2% reported more than 20 years of experience.
On analyzing the work setting distribution, 103 respondents (38.3%) were found to work in clinics and hospital settings. The hospital setting included multi-specialty hospital, super-specialty hospital, and general hospital set-up. Eighty-three respondents (30.9%) were from an Institution-based set-up, and 48 respondents (17.8%) practiced in a private set-up. There were 25 respondents (9.3%) who worked in schools. The other work settings included non-government organizations, neuro-rehabilitation centers, and community-based disability management centers, which constituted 3.7% of the total respondents. The respondents reported having exposure in dealing with individuals with various communication disorders such as child language disorders, voice disorders, fluency disorders, motor speech disorders, and swallowing disorders. Furthermore, 93 respondents (34.6%) reported having pursued additional dysphagia related certification courses such as FEES, fellowship in speech and swallowing rehabilitation in treating head and neck cancer, McNeil dysphagia therapy program, and MBSImp.
Following demographic response analysis, the percentage of respondents who work with individuals with dysphagia was calculated. Among the total respondents, 159 (59.1%) reported to have worked with individuals with dysphagia and were further directed to fill the subsequent sections of the survey. The results of the survey analysis of further sections were analyzed and are presented below.
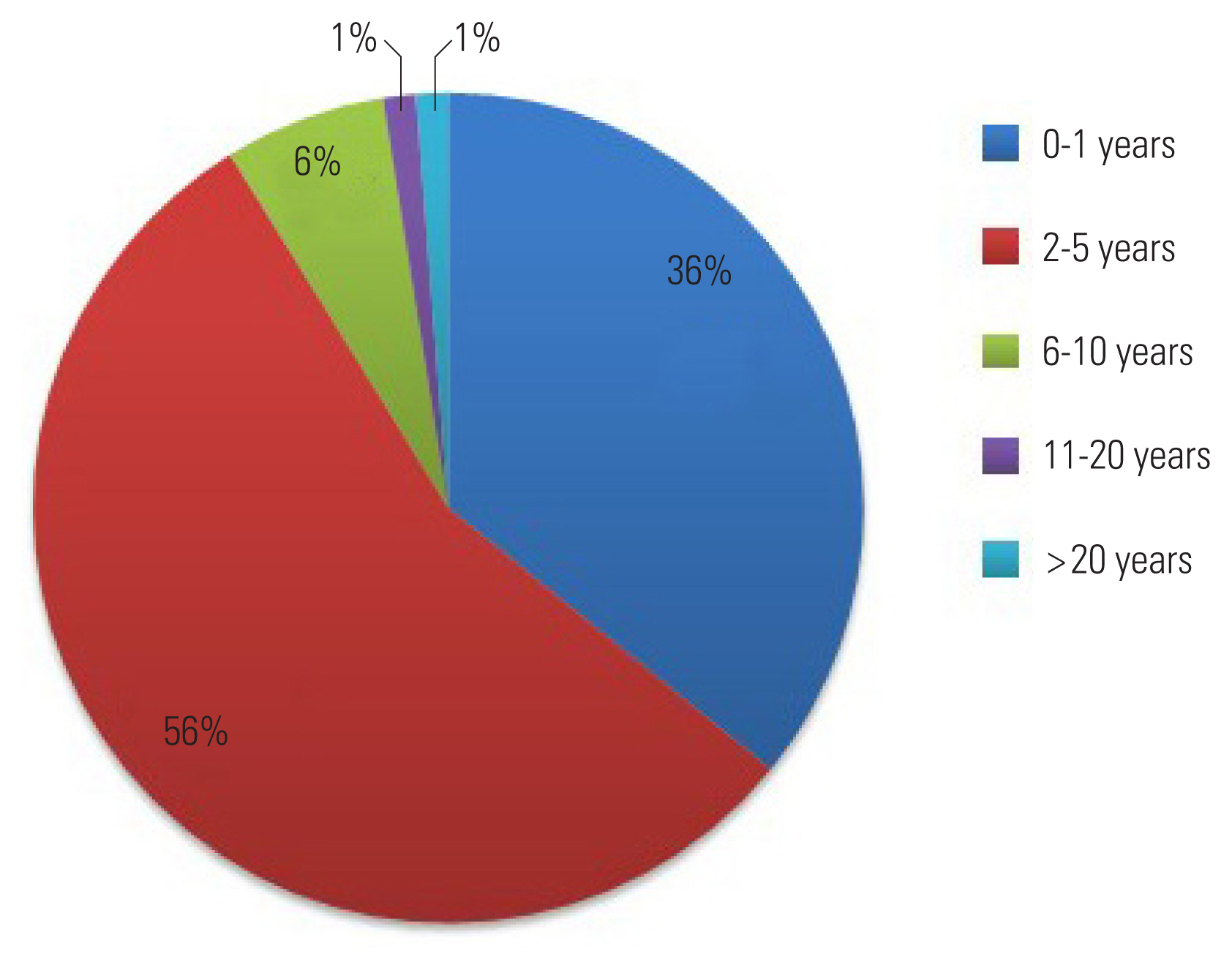
Part B: Dysphagia caseload characteristics
Amongst 269 respondents, 159 SLPs who had worked with individuals with dysphagia were eligible to participate in the subsequent sections of the survey. The percentage of SLPs’ work experience (in years) of working with dysphagia clients is provided in Figure 1. Majority of the respondents (n=88; 55.3%) had 2–5 years of experience, 57 (35.8%) of them reported to have 0–1 years of experience, 10 (6.3%) had 6–10 years of experience, and there were two respondents each who had 11–20 years (0.6%) and more than 20 years of experience (0.6%). The majority of the SLPs reported having seen adults (n=76; 48%) followed by geriatrics (n=35; 22%) and then children (n=30; 19%) with dysphagia. A considerable percentage of them had seen infants and newborns with feeding issues (n=18; 11%).
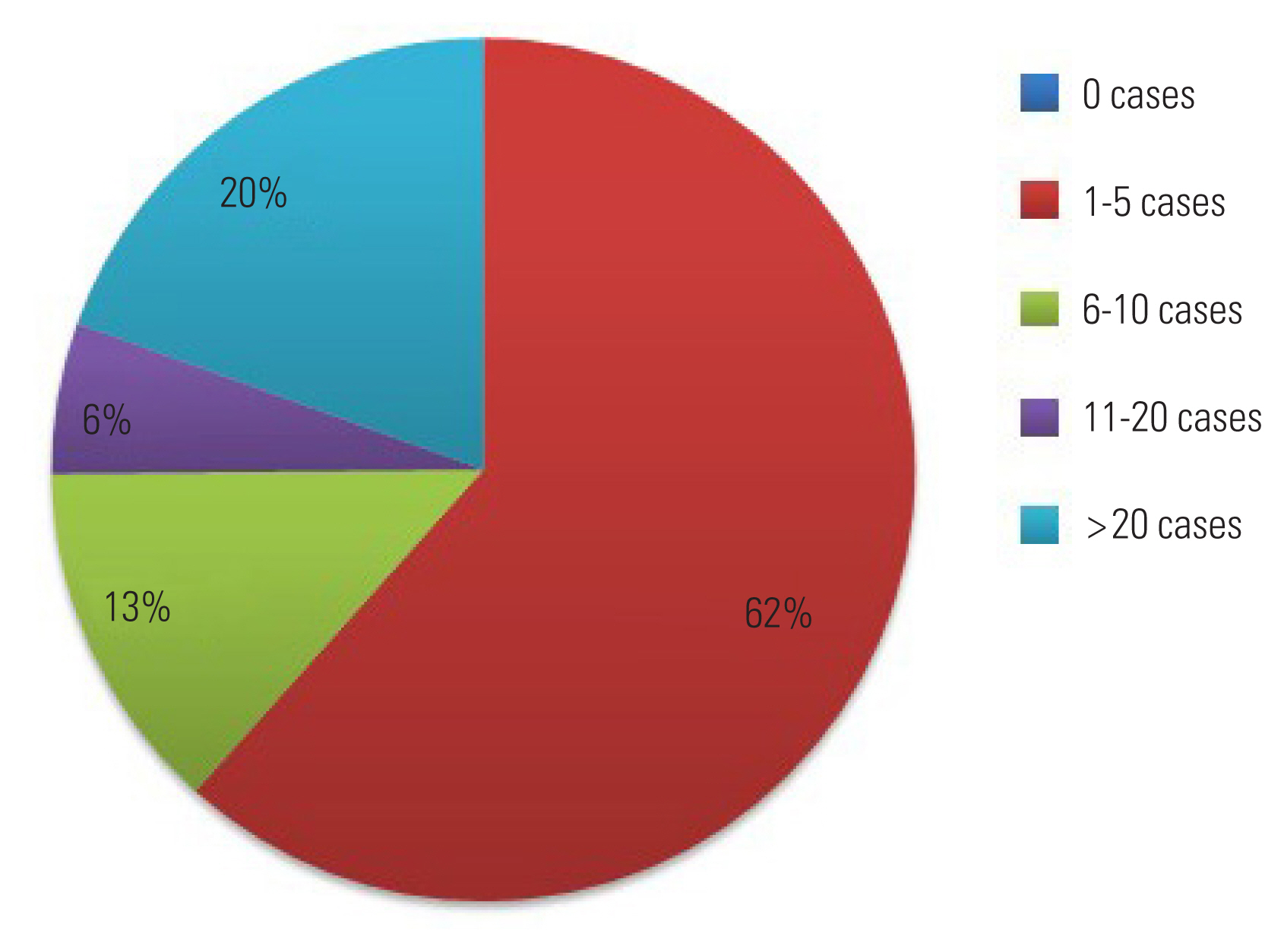
The respondents were asked about the caseload dedicated to dysphagia at their workplace in a span of a month. The percentages of dysphagia caseload as responded by the SLPs are provided in Figure 2. Most of the SLPs (n=98; 62%) assessed 1–5 individuals with complaints related to dysphagia every month; 31 SLPs (20%) evaluated more than 20 individuals with dysphagia in a month’s time; 21 SLPs (13%) reported that they evaluated 6–10 individuals with complaints of dysphagia, and nine respondents (6%) assessed 11–20 individuals with dysphagia every month. Twenty-four SLPs (15.1%) had undergone formal training to practice dysphagia services. A few training programs included, Langmore Foundation FEES course, Fellowship on Speech and Swallowing Problems in Head and Neck Cancer Patients, MBSImp, McNeill dysphagia therapy program, and VitalStim as reported. The respondents were asked if they worked in collaboration with a doctor at their work set-up. While 114 (71.7%) remarked that they worked with ENT doctors, 93 (58.5%) of them worked with Neurologists. In comparison, 38 (23.9%) respondents reported that they collaborated with maxillofacial surgeons, and 25 (15.7%) worked with PMR doctors. Contrarily, 38 SLPs (23.9%) worked independently with no inter professional collaborations.
Part C: Inclusion of SLPs in dysphagia team
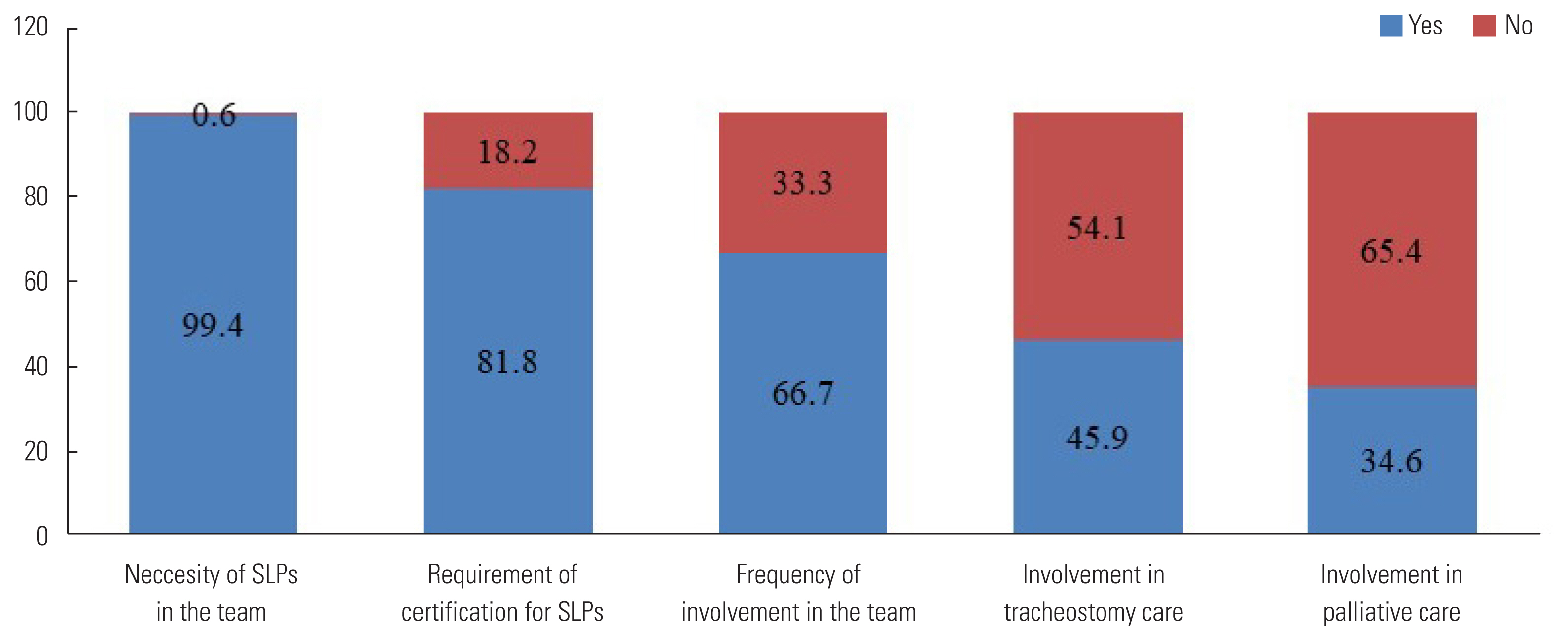
Concerning the necessity and involvement of SLPs in dysphagia rehabilitation, 158 of the total respondents (99.4%) asserted the necessity of SLPs in rehabilitating individuals with dysphagia, whereas one opined that there is no need for an SLP to be a part of the dysphagia rehabilitation team. Further, 130 respondents (81.8%) suggested that SLPs require formal and certified training to deal with individuals with dysphagia, and 29 of them (18.2%) reported that certification courses are not mandatory for managing individuals with dysphagia. However, 106 of the respondents (66.7%) reported that they were frequently involved in the dysphagia rehabilitation team. It was revealed that 53 SLPs (33.3%) remarked that they were not frequently called to be a part of the dysphagia rehabilitation team. Among all the respondents, 73 SLPs (45.9%) reported that they were involved in tracheostomy care and 55 (34.6%) were a part of palliative care. The responses obtained in Part C revealed SLPs’ perception of their necessity and involvement in dysphagia care which is expressed in terms of percentage (Figure 3).
Part D: SLPs’ knowledge and perception about their role in dysphagia team
Part D assessed fundamental knowledge of SLPs about dysphagia. The commonly associated conditions that the individuals with dysphagia presented to them included the following: difficulty in swallowing with slurred speech (36.4%), difficulty in swallowing with language disturbance (28.9%), difficulty in swallowing with degenerative diseases (22.3%), and difficulty in swallowing with deviant voice (12.4%). Almost all respondents knew that head and neck cancer treatment, traumatic brain injury, GERD, degenerative diseases, and tracheostomy causes dysphagia. When asked about the possible indications of dysphagia, SLPs reported choking during and after food consumption, anterior leakage (drooling), oral residue, increased duration of mealtime, multiple swallows, drastic weight loss, and pneumonia as the common symptoms of dysphagia. On asking for instrumental evaluation criteria, 58 (36.5%) respondents suggested recommending all the individuals who complain of dysphagia for instrumental evaluation. According to all respondents, the team of dysphagia rehabilitation should invariably include SLPs, ENT doctors or Laryngologists, Neurologists, and Dieticians. Further, 50% of the respondents opined that nurses, physiotherapists, and psychologists also should be a part of the dysphagia care team.
The survey assessed SLPs’ perception about their role in the assessment and management of individuals with dysphagia. Furthermore, they were asked about their involvement in various stages of assessment and management of individuals with dysphagia at their workplaces. Although the respondents perceived that their presence is essential in every assessment stage, such as clinical swallow examination, instrumental assessment, and counseling and management, a more significant proportion of SLPs (52.4%) were involved only during clinical swallow examination, followed by management (29.5%). Only 7.5% of them were engaged in instrumental assessment, and 10.6% of SLPs provided counseling services to individuals with dysphagia and their caretakers. Concerning the frequency of dysphagia therapy services, 95 (59.7%) SLPs provided one session of dysphagia therapy every day. Thirty-two SLPs (20.1%) delivered dysphagia therapy services once a week. Few of the respondents (25; 15.7%) reported that they provided dysphagia therapy for three sessions (during every meal time) in a day. Seven SLPs (4.4%) demonstrated the maneuvers to the caregivers. Regarding the referrals from other doctors, 35 (22%) SLPs reported that they always received referrals from doctors to evaluate individuals with dysphagia symptoms. Forty-six (28.9%) SLPs reported that they usually get referrals from concerned doctors; 33 (20.8%) SLPs received referrals only half of the time, 39 (24.5%) of them seldom received referrals, and 6 (3.8%) of them reported that they never received referrals from concerned doctors.
DISCUSSION
The present survey research aimed at assessing the knowledge and perception of SLPs’ about their role in the assessment and management of dysphagia. The survey questions were divided into four sections, and the results are discussed accordingly. In the first place, demographic responses were analyzed, and SLPs actively participated in the online survey research due to the increasing awareness and interest towards the field of dysphagia in the Indian scenario and apparent reasons of ease in the use of technology to fill out the online survey questions [10,11]. Given the workplace, most of SLPs worked in clinics followed by hospital setting. Among the total survey respondents, 59.1% of SLPs reported that they worked towards dysphagia care which indicates a positive professional advancement [12].
A majority of respondents had worked for 1–5 years in the field of dysphagia, followed by SLPs with 0–1 year of experience. Respondents with 6–10 years, 11–20 years, and more than 20 years of experience participated in the survey who can be considered competent SLPs working with dysphagia with good knowledge. Hence it may be inferred that the present survey included SLPs with a wide range of experience which is a good representation of practicing SLPs in India. As per the survey results, most of the SLPs working with individuals with dysphagia reported to have relatively less caseload (1–5 cases per month). This signifies reduced public awareness and need for advocacy to dysphagia practice by SLPs in India [11]. However, SLPs’ collaborations with concerned medical professionals such as ENT doctors, Neurologists, Maxillofacial surgeons, and PMR doctors have notably increased [11], which probably may increase the caseload in future practice. Among these, a significant proportion of SLPs reported their association with ENT doctors in case of mechanical dysphagia followed by Neurologists to evaluate and rehabilitate dysphagia of neurogenic origin. SLPs worked with maxillofacial surgeons to assess and manage feeding and swallowing issues in children with maxillofacial anomalies. Few SLPs reported that they worked in association with PMR physiatrists who implicitly deal with rehabilitation due to stroke, traumatic brain injuries. This highlights the expansion of SLPs’ association with dysphagia-related specializations for rendering better quality services for individuals with dysphagia.
SLPs did report a greater necessity of their services in rehabilitating individuals with dysphagia. Most of them also insisted on having a formal training or completed certification course related to swallowing and its disorders [7]. A formal education with hands on training to assess and manage dysphagia symptoms may substantially improve the speed and quality of recovery. However, formal training and ongoing workplace mentoring for advanced skill development has not been enforced in developing countries [7]. Most of the SLPs reported that they were not a part of dysphagia care team. This may be due to a lack of awareness among other health professionals about the role of SLPs, limited advocacy of clinical responsibilities of SLPs at their workplace, or lack of formal training in dysphagia rehabilitation. SLPs reported that they were not included in tracheostomy care where they may have a potential role to monitor swallowing-related issues such as removal of a nasogastric tube, initiating oral intake of food, which otherwise can turn fatal. Likewise, in palliative care, where individuals decline in their ability to communicate and eat even with assistance, SLPs assist to develop communication, cognitive, and swallowing strategies to add comfort and ease life quality [12]. This helps the expression and thus fulfillment of end-of-life goals and enhances overall care through interdisciplinary consultations. Although SLP is not a core member in most of the palliative care settings, there is an essential need to include SLPs in palliative care [13].
Concerning SLPs’ knowledge about dysphagia services, a majority of SLPs were aware of the signs and symptoms indicative of dysphagia. They also procured adequate knowledge on instrumental evaluation and its criteria, albeit only a few of them were involved in the instrumental assessment. SLPs opined that medical professionals such as ENT doctors, neurologists, dieticians, nurses, physiotherapists, and psychologists to be included in dysphagia care team [15]. Eventually, the study assessed SLPs’ perception about their role in the assessment and management of individuals with dysphagia. SLPs opine that their consultation is essential at all stages of assessment, such as case history, clinical swallow examination, instrumental evaluation, and management. Specifically, SLPs recommend their role in clinical decision making in terms of initiating oral intake of food, deciding consistency of bolus, demonstrating appropriate maneuvers and counseling. Despite their requirement in all the stages of assessment and management, SLPs are restricted to clinical swallow examination most of the time. In terms of intensity of dysphagia management, the frequency of therapy services varied from three sessions per individual per day to one session per week based on the severity of dysphagia and continued review referrals from concerned doctors. In continuation, there was an inconsistency in the frequency of referrals received by SLPs from concerned health professionals. While a few SLPs always received referrals, some of them revealed that they never received any referrals. Additionally, the respondents reported that doctors have limited awareness about the role of SLPs in dysphagia care, unavailability of full-time SLPs in dysphagia care team, and less number of SLPs with expertise in dysphagia as few reasons for not receiving adequate and necessary referrals from concerned doctors [6]. Overall, SLPs in India are making sincere efforts to gain knowledge and expertise in dysphagia care. However, guided training to SLPs and advocacy regarding the roles and responsibilities of SLPs among medical professionals are currently the absolute necessities in dysphagia service delivery.
CONCLUSION
SLPs’ knowledge and skill areas form the basis for assessing clinical competency in the specialized area of practice, Dysphagia care. Although SLPs who participated in the survey had substantial knowledge of dysphagia, it was found that they are not given adequate opportunities to work in the team of health professionals who work with individuals with dysphagia. Considering its preliminary nature, the present survey assessed knowledge of fundamental concepts related to dysphagia using limited questions. Besides, SLPs evaluating and providing treatment to individuals dysphagia should have a basic understanding of normal and abnormal anatomy and physiology related to swallowing function, signs, and symptoms of dysphagia, indications for dysphagia assessment, fundamental management issues including how to determine candidacy for intervention, as well as how to implement compensatory and rehabilitative therapy techniques, how to educate and counsel individuals with dysphagia and their care providers, or other supporting persons. They should also have a sound understanding of medical issues related to dysphagia. Hence, the above-mentioned issues may be addressed in future studies. Given a window of opportunity, SLPs make a significant difference in improving individuals’ quality of life with dysphagia. A qualified, trained, and experienced SLP can undoubtedly be a part of the dysphagia service providers’ primary team. For this, SLPs should be formally trained to assess and manage individuals with dysphagia, and various health professionals should be made aware of SLPs’ role in dysphagia services. If explicitly undertaken in the Indian scenario, these measures might result in an effective dysphagia service delivery by SLPs.
Supplementary Information
Notes
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest.
FUNDING
Not applicable.